Recent Research
Research articles
XMRV Update
- Details
- Last Updated: 24 November 2015 24 November 2015
There has been much controversy over whether the newly found XMRV virus infects humans and whether it is a causal agent of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS). The National Institutes of Health (NIH) has now undertaken a multi-center study to investigate why results in other studies differed so much, whether those studies actually duplicated the methods of the initial study, and whether positive study results were the result of contaminated reagents. It may take a year or more to learn the results.
Therefore, rather than posting every new article on the XMRV controversy, we are offering links that give a very comprehensive timeline and overall picture.
At Phoenix Rising, this link explains some of the history of XMRV.
The role of reactivated viral and bacterial infections in CFS/ME and FM, and the difficulty of their detection by normal antibody testing
- Details
- Last Updated: 25 November 2015 25 November 2015
We recommend this excellent research review on the role of reactivated viral and bacterial infections in the CFS/ME disease process. Dr.Kent Holtorf, MD, in an article for ProHealth, reviews 20 years of medical research pointing to the chronic reactivation of herpes viruses (EBV, CMV, HHV-6) and bacteria (mycoplasma, chlamydia pneumoniae, and Lyme disease), in ME/CFS and FM.
He also explains why the use of normal antibody tests, IgG and IgM, which normally detect the presence of a new and active infections do not identify chronic, reactivated infections in these illnesses. Moreover, these reactivated infections do not normally occur in the blood and sera, but in the cellular tissue (nerves, brain and white blood cells)—another factor making them hard to detect. He also identifies a number of markers that may indicate an underlying chronic infection in ME/CFS. Read the article.
25 Year Follow-up in Chronic Fatigue Syndrome: Rising Incapacity--Dr. Bell
- Details
- Last Updated: 25 November 2015 25 November 2015
Editors note: On April 16, 2011, Dr. David S. Bell was the keynote speaker at the Massachusetts CFIDS/ME & FM Association’s (MassCFIDS) continuing-education lecture series. The event was co-sponsored by the Massachusetts Department of Public Health at the Hinton State Laboratory Institute Auditorium. Dr. Bell, a retired pediatrician from upstate New York with intense curiosity, set out to find answers as to what made his young patients so ill during the cluster outbreak in the late 1980’s. Along the way, he became one of the world’s leading researchers on ME/CFS and one of only a handful of physicians who have been able to closely follow his patient population for decades. Dr. Bell has authored many research articles as well as leading books on Chronic Fatigue Syndrome.
by Joan Livingston
You've said it thousands of times: "I'm just fine, thanks." Very likely you've said it a few times today without stopping to think to yourself, "The hell I am." Part of living with a chronic disorder, after all, is becoming accustomed to feeling unwell.
Just how unwell patients actually are is a complex issue, and was a primary focus of Dr. David Bell's April 2011 presentation to the Massachusetts CFIDS/ME & FM Association. (His lively talk was well-attended, drawing participants from beyond the state's borders.) A national pioneer in treatment as well as research, Dr. Bell shared the results of his most recent study, an investigation of the current status of people who were diagnosed with ME/CFS twenty-five long years ago.
The study was limited to one group of patients—those who fell ill as children in Bell's rural hometown of Lyndonville, NY—but its provocative findings, on many patients' "rising incapacity," may well have implications for other patients.
Looking back at Lyndonville, NY
Dr. Bell previously published a paper on how well his pediatric-onset patients fared after 13 years, vs. the present timeline of 25 years. At the time of the earlier study, he reported that 80% of patients were "doing okay," with the other 20% remaining disabled. That conclusion was misleading, he now says, because the 80/20 figure created the impression that most patients had overcome the illness. "Doing okay," however, was not synonymous with being well.
About half of those in the "okay" group (or 40% of the total) were truly well. The other 40% still had significant symptoms and should therefore have been differentiated from the completely well and the completely disabled. Many thought they were "fine, thanks"; but they had not recovered.
What is recovery?
How recovery should or could be defined—by patients, by doctors, by society—has still not been resolved in ME/CFS, Bell said. "Is recovery the [total] absence of symptoms and a return to [entirely] normal function?" he asked, pointing out that many patients learn to deal with their limitations so well that they may not be perceived as ill.
The 40% of patients who weren't totally better often led what seemed to be normal lives, but "they had to be careful," Bell said. If they worked or exercised particularly hard, they had to allow themselves recovery time; using a common coping technique, they also tailored their calendars to avoid scheduling too many activities back-to-back. They couldn't work all day and then party at night, the way those who had recovered could.
The issue of recovery is multi-layered. There is no gold-standard lab test, as there are with other illnesses, to establish the absence (or presence) of ME/CFS. And people with chronic symptoms inevitably adapt to them; patients who cope effectively may inadvertently mask how ill they are, even to themselves. The problem is deepened by how well most patients look, and complicated further by the way many individuals, particularly medical professionals, continue to dismiss the reality of the illness.
Perception perplexity
Dr. Bell has long criticized doctors who see ME/CFS patients as psychiatric patients, rather than as physically ill. But MDs aren't the only ones with incorrect perceptions.
"For years I’ve been saying that people with CFIDS/ME aren't 'fruitcakes,’” he said. "But this is the one place where they actually are fruitcakes: They tend to be really confused about how sick they are."
The confusion can be profound; if a doctor as experienced as Bell can't define recovery, how can a patient be sure about his or her illness? Bell coined the phrase "health-identity confusion" to denote an inaccurate self-image, the result of "year after year after year of no answer."
The story of one Lyndonville patient illustrated the way doctors contribute to patients’ confusion. In diagnosing this woman, Dr. Bell referred her to three different specialists for evaluation. "One doctor said she had Hodgkin's, and had only a year to live. The second said she had Multiple Sclerosis, and had only 10 years to live." Bell paused, then delivered the kicker: "The third said she was a complete fruitcake and would never die.”
Little wonder, Bell remarked, that many patients will say, "I'm opting out of this system."
The long-term patients
In designing this and the earlier study, Dr. Bell gauged patients' signs and symptoms via an exhaustive list of objective measurements. The variables ranged from general concerns like fatigue to specific problems like headache, muscle pain, and lymph-node abnormalities. He studied physical functions, emotional symptoms, and mental functions (including memory and cognition) for an in-depth portrait of health status.
Patients were also asked, more subjectively, how well they thought they were. Remarkably, even when they knew they were participating in a medical study, many patients with severe symptoms overstated how well they were.
As with the 13-year study, to which this was a follow-up, 20% of the patients studied were fully disabled. (The study concentrated only on those who were still ill, not those who had recovered. "Those who got better stayed better," Bell asserted.)
Dr. Bell once again divided the unrecovered-but-not-disabled patients into two groups: persistent or chronic cases, and remitting ones. Patients in the first group were not "okay" in any way; they suffered from persistent symptoms, and functioned poorly.
People in the second group—the remitters—continued to experience many symptoms, but functioned well. Those in the control group (healthy individuals used for comparison to the ME/CFS study patients) had no symptoms and had normal functioning levels.
"Health-identity confusion" seemed to plague those in the remitting category. They considered themselves to be in good health, but all still had symptoms and abnormal lab tests indicating that something was physically amiss.
On the symptom scales, the remitting patients' scores fell about half-way between those of controls and those of chronic patients. A healthy person's score on one symptom might be zero (0), e.g., a chronic/persistent person's score might be 10; and a remitter's, in the middle at five.
Activity levels
Given the large list of factors that determine health, which ones were most important in determining whether someone was improving? Dr. Bell felt that the single most useful criterion in gauging overall well-being was how many hours someone spent engaged in upright activity each day: "hours of actually doing something, like work, school, or cleaning; not just sitting around, vegging-out watching TV."
Some people with ME/CFS log only one to five hours of cumulative activity a day, he said (those hours generally aren't consecutive; people might be active for only a few minutes at a time).
Healthy people, or controls, averaged 15 hours of daily activity; the remitting patients, about 13, fairly close to the level of "normals."
Upright activity was the best indicator of relative health in the survey; moreover, Dr. Bell felt it was the most reliable indicator of prognosis and recovery.
"When a person says they are getting better," he said, "it means they can do activities they couldn't do before." Although he posed his rhetorical question about how recovery should be defined, in his own practice he considered activity level and symptom severity in judging status and prognosis.
He warned that prognoses generally seemed poorest among those who remained bedridden for two or more years when they first became ill, and those who experienced particularly bad cognitive problems.
"The severity of the illness at onset is very predictive of the course the illness will take," he said. Worse outcomes were also common among patients who had a bout of infectious mononucleosis, separate from their ME/CFS onset.
Going downhill?
The findings of the 13-year and 25-year surveys were similar. With the exception of those who had recovered, however, no one seemed totally okay this time around.
Forty percent (40%) had essentially no symptoms and apparently normal activity, but they were not as well as controls. Among the 20% who remained disabled, many experienced increasing debility over time.
The remaining 40% (the remitters) still had symptoms, but their activity level was close to normal; that sounds like a good outcome, but in fact many ultimately experienced a return of symptoms or an erosion in activity level.
Dr. Bell called this aspect of his analysis "worrisome" (a patient might call it depressing). Many long-term patients not only didn't improve, but actually seemed to worsen over time.
That was true both of the sickest people, who were already disabled, and many who were recovering. "The bottom line is that people who don't fully recover seem to be getting gradually worse, and that makes me nervous,” Bell told a nervous audience.
That a person with a chronic illness could grow even more enervated was one disturbing prospect. That many people don't understand how sick they are was another one.
Dr. Bell gave the example of a mother "who thinks staying at home is her choice. She seems to believe she's basically lazy, which she isn't. But by not trying to enter the workforce, she doesn't have to deal with a lot of issues, including the disability question."
Bell said that some people simply denied they had symptoms, and that others chose to think they were hypochondriacs, rather than acknowledging they were sick.
While a good percentage of those in the Lyndonville study did recover for good, the continuing illness and vulnerability of the others raise vexing questions.
Is this group typical of all ME/CFS patients? It's important to keep in mind that these patients may differ from others in many ways beyond the fact that they got ill as kids; they lived in a small, rural town that experienced a local cluster outbreak in the mid-'80s, one whose triggers remain unknown.
Prime of life, rising incapacity
The trend toward "rising incapacity" in this study caused Dr. Bell to ruminate on how the illness could affect people during what should be the best years of their lives—which ME/CFS does already.
"At 40," he said, "you should be at the top of your profession, thinking, ‘Life is good.' At 60, you should be able to retire and to travel." Instead, many people in this group who became sick as children remained ill into middle age, with no indication they would enjoy better health as they got older.
Even those who were already disabled faced the prospect of even worse health.
An interesting side note: To complete this research, Dr. Bell contacted patients who had left the Lyndonville area, and his practice, at some point after their diagnosis and early treatment.
"When I called them, I asked, 'Have you told your current doctor that you have this illness?' A lot of them said something like, 'I'm not going to subject myself to that!"
This anecdote lent support to Bell's contention that many patients ultimately decide to avoid the health-care system altogether.
Looking forward
In addition to describing the 25-year study, Dr. Bell described early research into XMRV—a retrovirus recently linked to ME/CFS—and has already developed a new model of the illness, with XMRV as cause, to add to the existing library of "Bell disease models."
(Association members who attended earlier Bell lectures will find the new model similar to others describing the symptom cascade characteristic of the disease.) Dr. Bell actually studied the retrovirus family in the 1990s, thinking these were strong candidates for ME/CFS causation.
He described them this way: "Some viruses, like those in the herpes family, are relatively enormous. A retrovirus is a tiny, primitive thing, something more like our own normal 'junk' DNA. Retroviruses come from our distant past, and are inserted into our chromosomes."
Bell has contributed to early investigations of XMRV performed by the National Institutes of Health (NIH), but was cautious in his remarks. "I'm sorry that the subject is so far from resolution that I can't say much. There are all kinds of controversies about the work, like questions about whether the samples being studied have been contaminated in some way. The technical problems with XMRV are enormous, and I'd prefer not to go into detail about that here. These are issues that must be resolved by scientists; the good news is that smart people will figure it out."
XMRV research itself may be mired in controversy, but the basic concept of the virus as a ME/CFS trigger seems to be on firm footing. After Dr. Bell discussed the challenges ahead, MassCFIDS president Dr. Alan Gurwitt took the floor to say, "For too many years, the federal government failed us. The new people at the NIH and the Centers for Disease Control and Prevention (CDC) seem sincere, and we're hoping to see some real science now."
Oxidative stress
Bell tied the relatively new idea of XMRV to the concept of oxidative stress as another potential cause of ME/CFS. Oxidative stress is the term for bodily damage caused by free radicals (the "evil" molecules implicated in everything from simple infections to cancer and heart attack). Oxidative stress also reduces energy at the cellular level in the mitochondria, or energy factories, whose function is impaired in this illness (see our article Mitochondrial Dysfunction, Post-Exertional Malaise and CFS/ME). Bell described this part of his theory as follows:
- Oxidative stress causes aging.
- Patients have high oxidative stress.
- In patients, oxidative stress from ME/CFS is added to oxidative stress from aging, causing a double-whammy.
The notion of accelerated aging might ring a bell for patients. Bell stated that "Patients will say, 'I feel like I'm 95. My grandmother is 97, and she's more active than I am.’ This raises the question: Can you, at age 40, be a really old person?"
Anyone who's watched the labored gait of a 40-year-old patient, or seen one try to carry heavy packages, would answer yes.
Bell noted that XMRV could lead to infection with or without oxidative stress; if oxidative stress was involved, it would cause an increase in cytokines, disrupt the function of mitochondria, and injure natural-killer cells. Because all these phenomena are characteristic of ME/CFS, oxidative stress is a natural suspect in the causation of the disease.
Like other pathogens, XMRV is also a natural candidate, because the illness so often begins with an acute viral onset. "My bias is that this disease has a discrete cause," Bell said. Having seen so many people who were fine one day and sick the next, "I'm very biased about that; something happened that made patients sick," he said. Is it likely that many people have been infected with XMRV, and that some don't know it? Bell thinks it likely. "People are working on this like mad," Bell said, "but at this point they're working quietly."
Other highlights
Dr. Bell's review of the poor condition of some patients was sobering. More positive was the new work on XMRV and the oxidative-stress theory, because these might offer new insight into the illness and lead to more effective treatments.
Dr. Bell also had positive things to say about even the sickest patients. "I'd like to write a book about the incredible accomplishments of those with CFIDS," he said, citing the example of author Laura Hillenbrand; she wrote the best-selling book Seabiscuit while housebound (and mostly bed-bound). The acclaim she's received is unusual, but the way she chose to do something constructive, despite her limitations, was not.
“People learn how to treasure their good time and make something of it," Bell said. "They discover something that gives their life meaning."
Coping styles are important
“How people cope with this is unbelievably important," Bell went on. "And coping is an enormous issue in treatment."
He described three general ways in which patients respond to illness:
- denial
- tilting at medical windmills
- what might be called cheerful patience.
Some people simply ignore the fact that they're sick, he said—the patients who deny their symptoms, or chose to believe they're lazy, for example.
Others "run around and try every treatment out there." (Many patients go through a phase of frenetic activity, sampling alternative "treatments du jour" while also consulting doctors in every specialty. Some maintain this schedule indefinitely, while others burn out.)
Finally, Bell said, are the patients who remain patiently "open to treatment, waiting for that time [of a useful therapy] to happen. They've decided not to make themselves or their families miserable" by focusing obsessively on the illness over which they have so little control.
Condition at five years predictive?
Bell was asked about diagnosis, often a painfully long process, as too many Association members can attest. "My experience is that anybody who looks like they have CFIDS/ME at 3 months, will be diagnosable at 6 months.”
Once a patient receives a diagnosis, the next logical question—along with what treatment options are available—is, "How long will this thing last?" Bell sees five years as the point at which an individual's prognosis can often be established.
"If someone's condition isn't improving after five years, if things aren't changing, they're probably going to stay there," he said. "If they're really bad off then, their situation will likely become one of those nightmares we've all heard about." Bell has seen patients improve after the five-year mark, but in his practice, dramatic improvements after that point were not common.
While the focus of the talk was on long-term illness, rather than on patients who recovered or improved, Bell spent some time talking about the patients who saw "good results." He said he had not seen anyone recover as a direct result of physical therapy, but cautioned that he had trouble differentiating the effects of exercise from recovery in general.
There are many types of physical therapy. Stretching joints may be important for someone who is developing contractures but, Dr. Bell said, stretching “is not going to increase exertion that much. If you’re talking about an exercise therapy where you are out and jogging around the block, you have to use common sense.”
Patients must judge for themselves how much exercise they can tolerate (if any), watching carefully for post- exertional malaise. Dr. Bell stated that “Sometimes doctors have no way of assessing this based upon a physical exam.”
Asked whether he'd seen any other approaches that correlated with better results, he said no. "There are lots of people who eat terribly, don't exercise, and generally don't take care of themselves who get well anyway," he said.
He was talking not about treatments, but about personal lifestyles, which—at least in his experience—just didn't seem to make much difference in recovery rates.
Whether ME/CFS is casually contagious (can be spread through kisses, coughs, or sharing kitchen utensils) is a perennial question. With the introduction of a new virus, XMRV, audience members once again asked about contagion. "My personal belief is that the disease could be casually contagious only in the first six weeks," Bell said, "but you don't tend to see people transmitting it to anybody else. Transmission would be extremely unlikely with XMRV, because of the low viral load."
The future
Also on the topic of XMRV, Dr. Bell suggested the possibility that many people may have been exposed to this virus without developing symptoms. He mentioned one patient who didn't have ME/CFS, but had suffered through two years with mononucleosis when she was in college; she tested positive for XMRV. He said he wouldn't be surprised if it turned out that some people who were fine at age 20 became symptomatic as they aged, perhaps developing ME/CFS at age 40 or later. This is another subject for future research.
Bell concluded his remarks by saying, "We should be much further along in our understanding of the illness than we are at present." That we are as far along as we are is due in no small part to Dr. Bell’s persistent work in the face of untold challenges.
Lecture by Dr. David Bell, April 16, 2011
- Details
- Last Updated: 19 October 2021 19 October 2021
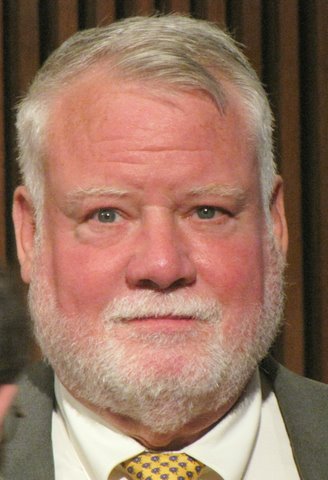 Dr. David Bell is arguably one of the most respected and appreciated physicians among patients in the CFS/ME community. He is a pioneer clinician and researcher who was first introduced to the debilitating effects of this disease during an outbreak in Lyndonville, NY, in the 1980’s. Although now retired from his medical practice, he continues to participate in studies and research on this complex and difficult illness.
Dr. David Bell is arguably one of the most respected and appreciated physicians among patients in the CFS/ME community. He is a pioneer clinician and researcher who was first introduced to the debilitating effects of this disease during an outbreak in Lyndonville, NY, in the 1980’s. Although now retired from his medical practice, he continues to participate in studies and research on this complex and difficult illness.
The Massachusetts CFIDS/ME & FM Association was pleased to host Dr. Bell at an event co-sponsored by the Massachusetts Department of Public Health at the Hinton State Laboratory Institute Auditorium on Saturday, April 16, 2011. Attendees included patients, family members, and medical practitioners from Massachusetts and several surrounding states.
In his lecture, "25 Year Follow-up in Chronic Fatigue Syndrome: Rising Incapacity," Dr. Bell spoke about his 13 year follow-up study paper and his more recent 25-year follow-up research. He highlighted his findings about “health-identity confusion” and “rising incapacity” among surveyed subjects. He also spoke about oxidative stress as another potential contributing factor in the disease. While he focused on long-term illness, he also spent time talking about the patients who had good results.
An enthusiastic Question and Answer period followed the lecture, and in the opening remarks Dr. Bell discussed the early research into XMRV and the current controversy surrounding this discovery. Questions from the audience touched on a variety of topics including the likelihood of viral or retroviral involvement, individuals who present with chronic EBV, the possibility of casual transmission in the first six weeks of the illness, the effects of IV saline and the benefits of B-12 treatments, the use of Provigil, the future of XMRV research, and more.
View the video of the lecture (55 minutes)
View the video of the Q&A (42 minutes)
"25 Year Follow-up in Chronic Fatigue Syndrome: Rising Incapacity"
(an article summarizing Dr. Bell’s remarks for those who prefer a written format)
Mitochondrial Dysfunction, Post-Exertional Malaise and ME/CFS
- Details
- Last Updated: 15 March 2021 15 March 2021
Editorial notes
-
The article below is germane to ME/CFS patients who have post-exertional malaise. This is a requirement for meeting the 2003 Canadian Definition of ME/CFS and the proposed definition in the Institute of Medicine Report Guide for Clinicians in 2015. The majority of ME/CFS patients meeting the 1988 CDC criteria have this symptom. Far fewer of those meeting the 1994 CDC or other definitions will have this symptom. A patient who lacks post-exertional malaise as described below does not have mitochondrial dysfunction. This type of exhaustion is unique to mitochondrial problems.
-
This article is intended to be read by lay readers as well as health care providers. Thus, we will sometimes explain medical terms. We will use the term ME/CFS for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome/Chronic Fatigue and Immune Dysfunction Syndrome in deference to our health-care provider readers.
-
Mitochondrial dysfunction is only a partial cause of the fatigue most ME/CFS patients have. It has been well documented that there is an abnormal increase in cytokines (chemicals released by the immune system) in ME/CFS patients following mild exercise. This causes another type of fatigue on top of the mitochondrial dysfunction fatigue discussed below. Cytokines in general, without the exercise trigger, can cause fatigue. There are probably additional causes of fatigue (such as orthostatic intolerance) as well.
-
The author of this article is an elected member of the New York Academy of Sciences, and Sigma Xi: The Scientific Research Honor Society, as well as other scientific societies. She is also a past member of the board of the Massachusetts CFIDS/ME & FM Association.
The role of mitochondria in cellular function
Except for red blood cells 1, every cell of the human body contains mitochondria—which are cellular bodies that manufacture the energy needed by the cell in order to function. The energy is essentially created by the conversion of ATP (adenosine triphosphate) to ADP (adenosine diphosphate). Thus, a molecule of adenosine with three phosphate molecules attached becomes adenosine with two phosphate molecules attached, and energy is released during the reaction. In a reverse chain of chemical reactions, ATP can be created from ADP or from AMP, which is adenosine with one phosphate molecule attached. All of these reactions involve multiple chemicals and enzymes. The ATP is initially derived from either carbohydrate (in the form of glucose or glycogen (a form of glucose stored in cells)) or fatty acids. 2
Glycolysis is the metabolic pathway in mitochondria that converts glucose/glycogen into pyruvate and hydrogen. The pyruvate is transformed into acetyl-coenzyme A (acetyl –CoA). If there is sufficient oxygen, the acetyl-CoA then undergoes the Krebs cycle (also called the citric acid cycle). The biochemistry of the Krebs cycle is very complex. 2, 3, 4 We will not go into it here. The rate of the Krebs cycle transformations determines how much ATP is ultimately generated. 3 The Krebs cycle involves vitamin B-1 (thiamine), vitamin B-2 (riboflavin), magnesium, and malate (from malic acid), which has implications for treatment of mitochondrial disorders. 2
As a result of the Krebs cycle and what is called the Electron Transport Chain, ADP is transformed into ATP. (This transformation of ADP into ATP using oxygen is called oxidative phosphorylation.) Reactive oxygen species (ROS) build up as a byproduct and these damage mitochondrial membranes (inner and outer), cellular RNA, cellular DNA, proteins made by the cell, and cellular membranes .4, 5 Damage caused by ROS is called oxidative stress. ROS can cause apoptosis of the cell (cellular suicide.) 4, 5, 6, 7
If there is not sufficient oxygen, then less ATP is created and lactate builds up as a byproduct. To quote from Wikipedia 8 (which is an exposition of material in Science 9):
“When the energy in ATP is utilized during cell work (ATP hydrolysis), protons are produced. The mitochondria normally incorporate these protons back into ATP, thus preventing buildup of protons and maintaining neutral pH. If oxygen supply is inadequate (hypoxia), the mitochondria are unable to continue ATP synthesis at a rate sufficient to supply the cell with the required ATP. In this situation, glycolysis is increased to provide additional ATP, and the excess pyruvate produced is converted into lactate and released from the cell into the bloodstream, where it accumulates over time. While increased glycolysis helps compensate for less ATP from oxidative phosphorylation, it cannot bind the protons resulting from ATP hydrolysis. Therefore, proton concentration rises and causes acidosis.”
We will discuss the consequences of this below in the section on the characteristics and consequences of mitochondrial dysfunction fatigue.
When there is insufficient glucose/glycogen for the mitochondria to synthesize ATP, then fatty acids are used as a fuel source. This involves the release of fatty acid from fat cells into the blood stream, “activation” and transport of the free fatty acids into the mitochondria of a cell, and the break-down of the fatty acid into acetyl-CoA, which ultimately yields ATP. This last step is called beta-oxidation. 2, 10 Unfortunately, the process of the activation and transport of long chain fatty acid into mitochondria involves breaking down ATP into byproducts and transporting the relevant byproduct (acyl-CoA—which isn’t the same as acetyl-CoA) via what is called the carnitine transport system. 2, 10, 11, 21 Thus ATP has to be used to transport a byproduct of fatty acid into the mitochondria in order to create more ATP.
Once in the mitochondria, the acyl-CoA is transformed into acetyl-CoA as part of beta-oxidation. After acetyl-CoA is created, it enters the Krebs cycle and the process of creating ATP is like that for creating ATP from glucose using oxygen. Involved in the transport system and beta-oxidation are acetyl-carnitine, co-enzyme Q-10, biotin, and vitamin B-12, which has implications for the treatment of mitochondrial disorders. 2, 10, 11, 12
Most types of cells can utilize fatty acid as a fuel except for the cells of the brain. 10 When the cells of the liver utilize fatty acid in their mitochondria, they generate chemicals called ketone bodies. The ketones then enter the blood stream. All cells of the body, including brain cells, can use ketones as an alternate source of energy. 10
Generally speaking, cells prefer to use glucose as a fuel, under oxygenation. During fasting, fatty acids and ketone bodies are more important energy sources for most cells, with the idea that the glucose available is saved for brain cells. 10 The situation in skeletal muscle cells is more complicated. The choice of fuel source is largely determined by exercise intensity and duration. As exercise intensity increases, the use of glucose/glycogen intensifies. However, at low intensity or moderate exercise, fatty acid is the preferred fuel .10, 11 As for the heart, fatty acids are the preferred fuel for 60-90% of its energy needs. 14
Illnesses with mitochondrial dysfunction, including the case for ME/CFS
The first appearance of a mitochondrial disease in the medical literature was probably the description of adult onset blindness by Theodur Lebur in 1871. 15 (This is now known as Leber's Hereditary Optic Neuroretinopathy (LHON).) 16 However, the existence of mitochondria in cells was still in the process of discovery and their role in the illness was not known. The existence of mitochondria in cells was discovered over time from 1857-1886. 17 The elucidation of their function and the role of ATP in cellular energy generation took most of the 20th century (1912-1997). 17 In 1962, Luft’s disease (which involves hypermetabolism and elevated core temperature) was the first proposed mitchondrial disease. 18 It wasn’t until 1989 that the mitochondrial and genetic bases of LHON and Luft’s illness were confirmed. 18 The first discovery of pathogenic mitochondrial mutations in DNA was in 1988. 15 The role of inherited genetic mitochondrial defects in mitochondrial myopathies was only elucidated in the late 1980s and 1990s. 17 The role of inherited genetic mutations in fatty acid beta-oxidation enzymes started to be elucidated in the 1970s and 1980s. Many aspects are still unknown. 10
While many inherited genetic mitochondrial disorders occur in the mitochondria of all cells in the body, some are limited to specific cell sites, such as the eye, motor neurons (as in Lou Gerhig’s disease or amotrophic lateral sclerosis), skeletal muscle, or brain (as in Huntington’s disease). 10, 11, 12, 13, 14, 15, 19, 20
The role of acquired mitochondrial dysfunction in common diseases has only begun to be elucidated the last fifteen years or so. It is now known that dysfunctional mitochondria play an important role in diseases of the brain such as Alzheimer’s, and Parkinson’s. 19, 20, 21 Type-2 diabetes mellitus is also known to be an acquired mitochondrial dysfunction disease of the mitochondria in skeletal muscle and the pancreas. 3, 6, 22, 23, 24, 25, 26, 27, 28, 29
ME/CFS patients are not immune to the type-2 diabetes epidemic. So, we will note that in addition to any mitochondrial problems stemming from ME/CFS, patients also having metabolic syndrome or type-2 diabetes are having trouble with the mitochondrial problems from these conditions as well. Fewer and smaller-sized mitochondria are found in the skeletal muscle of metabolic syndrome or type-2 diabetic patients. 28 This is significant because normally 67% of the volume of skeletal muscle cells is occupied by mitochondria, compared to 20-30% of cardiac muscle cells. 28 There is diminished electron transport activity in mitochondria of skeletal muscle of diabetics that can’t be explained just by the diminished numbers of mitochondria. 3, 28 Fatty acids tend to accumulate in the cells of skeletal muscle in type-2 diabetes and this leads to reduced mitochondrial oxidative capacity. 3, 28 There is clearly a defect in the ability of skeletal muscle to oxidize fatty acids. 27 It is also the case that evidence exists of decreased mRNA (messenger RNA) expression of several genes associated with oxidative phosphorylation in first degree relatives of type-2 diabetics. 27 For a more detailed overview of the role of mitochondrial dysfunction in type-2 diabetes, see reference #27.
Since a number of ME/CFS patients are known to be also hypothyroid, hyperthyroid or have polycystic ovary syndrome (PCOS), it should be noted that insulin resistance and mitochondrial dysfunction in skeletal muscle play roles in these conditions. 29 In the cases of both hypothyroidism and hyperthyroidism, there are decreased glycogen synthesis, down-regulated intracellular glucose catabolism, altered blood flow, and decreased muscle oxidative capacity in skeletal muscle. 29 In PCOS, it is the case that there is decreased glycogen synthesis and impaired mitochondrial oxidative metabolism in skeletal muscle. 29 Thus ME/CFS patients with one or more of these additional conditions will have increased mitochondrial dysfunction in skeletal muscle, compared to ME/CFS patients who just experience post-exertional malaise.
The evidence that ME/CFS is at least in part an acquired mitochondrial dysfunction disease of skeletal muscle is now quite strong. 30, 31. 32, 33, 34, 36, 37, 38, 39, 41, 42, 43, 44, 45 We could find only one study that looked at mitochondrial function in other types of cells in CFS/ME. 40
Vermeulen et al. 30 found that in two exercise tests 24 hours apart, ME/CFS patients reached an anaerobic threshold and maximal exercise capacity at a much lower oxygen consumption than controls. This discrepancy was worse on the second test. The researchers concluded that this demonstrated an increase in lactate production and decrease in ATP production compared to controls. They did other tests that seemed to indicate that the oxidative phosphorylation occurring in both ME/CFS patients and controls was the same. So, they concluded that the dysfunction involved another pathway other than oxidative phosphorylation. (Other studies don’t agree with this conclusion.)
Kennedy et al. 31 found increased markers of oxidative stress in ME/CFS patients and that the magnitude of the increase was correlated to the symptoms of post-exertional malaise. Paul et al. 32 found that both ME/CFS patients and controls showed a decrease in voluntary muscle contractions during exercise consistent with fatigue following maximum voluntary contractions. Thus the researchers concluded that even though the force of the contractions were always less in the ME/CFS group, the patients were working to their maximum capacity. ME/CFS patients were unable to recover their pre-exercise force of contraction after a 200-minute recovery period that worked for healthy sedentary controls. In addition, muscle contraction force was even less 24 hours after the exercise than immediately after the exercise for the ME/CFS group. The researchers concluded that this was consistent with mitochondrial dysfunction.
In 1984, several years before CFS was defined in the U.S, Arnold et al. 33 found that using 31P nuclear magnetic resonance they could demonstrate an abnormal rise in intracellular acidity in the exercised forearm of a British patient with post-viral fatigue syndrome (ME). Because the rise was out of proportion to associated changes in high-energy phosphates, they concluded it demonstrated an excessive lactic acid formation due to an acquired disorder of metabolic regulation. In 1991 the Behans reported finding mitochondrial abnormalities in the biopsies of skeletal muscle of 50 ME patients. 34 (It should be noted that the patients studied by the Behans had ME after infections of skeletal muscle with enteroviruses such as Coxsackie.) Other studies have not found structural abnormalities in mitochondria. 35
In two studies, the Plioplys found that there were no obvious structural changes to mitochondria in skeletal muscle biopsies of ME/CFS patients 35, but the ME/CFS patients had statistically significant lower levels of serum total carnitine, free carnitine and acylcarnitine compared to healthy controls. 36 They concluded this was due to dysfunctional mitochondria. They also found a statistically significant correlation between lower serum total and free carnitine levels and worse clinical symptomatology. 36 Earlier, Kuratsune et al. 37 had discovered that deficiencies of serum acylcarnitine had statistically significantly correlated with worsened fatigue symptoms in CFS/ME patients, but the researchers had not measured total and free carnitine levels.
Using ME/CFS patients identified by the 1994 CFS case definition (which is broader than the 1988 or Canadian definitions of CFS), Lane et al. 38 identified two subgroups of CFS patients. One group had an abnormal rise in lactate following exercise (which they called the SATET+ve group) and the other did not (SATET-ve). They did phosphorus magnetic resonance on the forearm muscles of 10 ME/CFS SATET+ve patients, 9 ME/CFS SATET-ve patients, and 13 healthy controls. There were no differences in spectra at rest for the three groups, but after exercise the ME/CFS SATET+ve patients showed a significant increase in intracellular acidity compared to the other two groups. The ME/CFS SATET+ve patients also showed a significantly lower ATP synthesis rate during recovery from exercise than the other two groups. The researchers concluded these ME/CFS patients showed impaired oxidative phosphorylation, but the others (SATET-ve) did not.
In the book Mitochondria in Pathogenesis, Chazotte 39 gives a detailed overview of the evidence for mitochondrial dysfunction in ME/CFS as of 2000. He observed:
“Thus there is ample clinical evidence to suggest a role for mitochondrial dysfunction in many different tissues and cells in CFS, which could give rise to many of the symptoms. Whether this role is due to a specific mitochondrial defect, perhaps in genetically susceptible individuals, or is an effect of some other problem such as altered cytokine levels that in turn affect mitochondrial function, needs investigation. Due to the difficulty in obtaining human specimens in sufficient quantities per specimen for biochemically based studies of mitochondrial function, there are few (and no detailed) studies of mitochondrial function in CFS patients.” 39
Myhill et al. 40 undertook to rectify this lack of biochemically based studies and examined blood neutrophils (a type of white blood cell) of 71 ME/CFS patients and 53 healthy controls to obtain five numeric measurements of mitochondrial function, called the ATP profile test. The ME/CFS patients were ranked on the Bell CFS Ability Test (developed by Dr. David Bell) to give a scale measurement of ME/CFS severity from 0 to 10 (with 0 being “constantly bedridden with severe symptoms and unable to care for himself/herself”). The ME/CFS patients were in the “very severe” (25 patients), “severe” (21 patients) and “moderate” (25 patients) ranges on the Bell scale.
In some of the five measurements, there were ME/CFS patients who had above the minimum (but below the average) measured in the controls. The three of the most severely ill patients had one value each within the low normal range for controls, but the other four values were well below the minima for the controls. When the number of the five measurements that were below the minima of the healthy controls was taken into account by the researchers, on average the “very severe” patients had 3.7 measurements totally below the normal ranges, “severe” patients had on average 3.5, and the “moderate” patients had on average 2.2 of the five measurements below the normal ranges.
The researchers pointed out that if they had only measured one factor instead of five, significant numbers of the patients would have been classified as “normal” (albeit usually very low normal) for the factor. They stated, “For example, if only ATP had been measured, 28% of all the patients would be classified as normal, and if only Ox Phos had been measured, 32% of the ‘very severe’ patients would be classified as normal.” 40
Finally, the researchers concocted a Mitochondrial Energy Score for each patient using the five factors, which they said measured the overall mitochondrial energy-producing efficiency of the neutrophils of the study participants. Only one of the 71 patients had a Mitochondrial Energy Score above the minimum for the healthy controls. That patient had a Bell CFS Ability Score of 7, but also had two of the five factors below the minima for the healthy controls. Since the CFS Severity Score had been computed first for the patients, the researchers looked at predicting CFS severity from the Mitochondrial Energy Score.
They concluded that mitochondrial dysfunction is a major risk factor for severity in ME/CFS. However, they also noted that since they measured the ATP factors only in neutrophils, conclusions could only be reached concerning adverse effects on the function of the immune system, not in skeletal muscle. The researchers observed:
“Our observations strongly implicate mitochondrial dysfunction as the immediate cause of CFS symptoms. However, we cannot tell whether the damage to mitochondrial function is a primary effect, or a secondary effect to one or more of a number of primary conditions, for example cellular hypoxia or oxidative stress including excessive peroxynitrite." 40
Characteristics and consequences of mitochondrial dysfunction fatigue in skeletal muscle
Those who have mitochondrial dysfunction of the skeletal muscle can experience two main types of fatigue. One is the result of increased acidosis inside the muscle cells and has as a marker increased lactate in the blood. This is a result of muscle cells trying to create ATP when there is insufficient oxygen. Endurance athletes (such as marathoners) can experience this type of fatigue. They refer to it as “hitting the wall." 8, 9 It is also referred to as “metabolic fatigue.” 46
The second type of fatigue is the result of a large build-up of Reactive Oxygen Species (ROS) and depletion of ATP in the muscle cells. As far as we can determine from a careful search of the medical literature, this second type of fatigue is unique to patients with known inherited genetic mitochondrial diseases of skeletal muscle, AIDS patients undergoing treatment with antiretroviral drugs (who have severe mitochondrial dysfunction), 47 and ME/CFS patients experiencing post-exertional “malaise.” It is this second type of fatigue that has the most permanent serious consequences for patients.
The first type of fatigue, metabolic fatigue, feels like a burning, dull aching weariness in muscles. The affected muscles feel stiff and affected limbs feel heavier and heavier, as the ability of the muscles to contract declines. 49 The increased acidity in the muscle cell lowers the sensitivity of the contractile apparatus to calcium Ca2+. It is unclear what exact role lactic acid has in this process, but increased lactate in the blood is a marker for this type of fatigue. 46
As mentioned in the preceding section, a subgroup of ME/CFS patients have an abnormal rise in lactate with minor exercise and a very slow recovery from this condition. 30, 32, 35, 38, 48 It is not unusual for these patients to require 24-48 hours or more of bed rest to fully recover. Even in healthy people, delayed onset muscle soreness (DOMS) occurs with severe muscle tenderness as well as loss of strength and range of motion, usually reaching a peak 24 to 72 hours after the “extreme” exercise event that caused the excessive lactate in the blood. 49 (Healthy people don’t have to retire to bed to recover, however.) Exercise physiologists still do not understand why DOMS occurs, but most research points to actual muscle cell damage and an elevated release of various metabolites into the tissue surrounding the muscle cells. 49 These lead to an inflammatory repair response that lasts a couple of days in healthy people. 49 How long it lasts in ME/CFS patients who have excessive lactate after very little exercise is unknown. For some ME/CFS patients, just standing up for 10 minutes is enough to create this problem. It should be noted that excess lactic acid is now known to be neurotoxic, so continual problems with this could lead to the death or damage of motor neurons in skeletal muscle. 50
The more serious type of fatigue is the one resulting from excessive build-up of ROS in the muscle and depletion of ATP. This type of “fatigue” is extreme prostration that occurs 8 or more hours after exercise (or what passes for “exercise” in ME/CFS patients and would be considered normal activity by healthy people.) Patients feel a deep, whole-body weariness and feel the necessity to lie still and not move due to extreme fatigue. Trying to even turn over in bed requires a great deal of painful effort of will. In addition, patients feel very sore all over their bodies. ME/CFS patients often describe this as feeling being beaten up and run over by a Mack truck or bus. The term post-exertional “malaise” seems pathetically inadequate as a descriptor of this feeling.
Mitochondrial specialist Dr. Donald Johns 51 has warned that when a patient feels this way, it is very important to listen to his/her body. The extreme fatigue feeling is from depletion of ATP and the beaten-up/run-over feeling is from excessive ROS that not only did permanent damage to muscle cells, but also is still doing damage. Thus, it is essential to stay in bed and move as little as possible until the condition improves—even if that takes days. The best thing to do is for the patient to try to avoid getting into this condition in the first place by pacing and staying inside his/her “energy envelope.” This is not so easy to do at times, however.
ROS produced in the mitochondria damage mitochondrial DNA, for instance. 3 This leads to alterations to the polypeptides encoded by the DNA. A decrease in electron transfer then ensues, but electron transfer is needed for generation of ATP. Thus, more ROS are produced in a vicious circle of oxidative distress and energetic decline. 52 Mitochondrial DNA damage also results in daughter cells that are mutated and in cellular apoptosis. 4, 5, 6, 7, 28
Muscle inflammation and oxidative stress are now known to play an important role in muscle atrophy. 53 In addition, many ME/CFS patients have a low-grade fever, which means they have high levels of interleukin-1 (IL-1). 54, 55 IL-1 is known to cause muscle catabolism (muscle destruction). 54, 55 So ME/CFS patients with high levels of ROS and low-grade fevers can expect noticeable destruction of skeletal muscle with difficulty in replacing it.
ROS generated from mitochondria also damages proteins and lipid in membrane components for mitochondria membranes and cellular membranes. This results in more mitochondrial dysfunction and cellular apoptosis. 4, 5, 6, 7, 28
All in all, ME/CFS patients need to try to avoid post-exertional malaise as much as possible in order to avoid permanent damage and permanent adverse changes to skeletal muscle.
Treatment
Living in the “energy envelope”
Mitochondrial specialists advise conserving energy to minimize the two types of fatigue. 51 ME/CFS specialists advise acknowledging the finiteness of energy for each patient for each day. Some call this the “energy envelope.” 59, 60, 61 Unfortunately, the energy and ability to function will vary for the patient from day to day. Especially if more is done one day, less will have to be done on following “recovery” days. Thus, the patient needs to make constant cost/benefit judgments about doing activities that use energy. There will be times that a patient decides that the psychological and emotional benefit of an activity outweighs the physical cost. That is acceptable, as long as the patient attempts to limit the physical damage that follows the activity and recognizes the recovery time that will be necessary. 63 We consider this acceptable since it is now known that most patients either do not recover, or don’t recover for years, if not decades. 62, 64 , 65 It is psychologically important for a patient to have some daily activity that creates a vestige of joy and psychological well-being, and not put everything “on hold” awaiting a recovery that might not come. 63
Supplements to treat mitochondrial dysfunction
Other than metformin, angiotensin II receptor inhibitors, and angiotensin converting enzyme inhibitors that help with the mitochondrial dysfunction of type-2 diabetes, there are no known pharmaceuticals for mitochondrial dysfunction. 27 Thus treatment consists of pacing (as described above) and over-the-counter supplements. Physicians will have to adjust dosages for the individual patient, especially keeping in mind that ME/CFS patients tend to be very sensitive to pharmaceuticals and supplements. It should be noted that very few side effects, if any, are known for the supplements below and very few interact with pharmaceuticals. More information about side effects, maximum safe dosages and interactions with pharmaceuticals can be found in the PDR for Nutritional Supplements 56 and on our website in "Review of Nutritional Supplements Used for ME/CFS/FM."
When we give dosages, we are usually quoting those given by mitochondrial specialists (which tend to be higher than those suggested by ME/CFS specialists). It is still not known what levels in the blood are needed to cross the cellular membrane and enter the mitochondria. 57, 58 Besides pacing, treatment is broken up into the categories of improving the function of mitochondria, antioxidants to help prevent damage from ROS, and recovery from excess acidosis and post exertional malaise.
Mitochondrial Function
- Magnesium (up to 600 mg a day 2, 71, 76, 80, 81 (Blood levels must be monitored periodically for patient safety))
- Co-enzyme Q-10 (100-200 mg three times a day) 27, 50, 51, 58, 66, 67, 68, 69, 72, 79, 80, 81
- Acetyl-l-carnitine (500-1000 mg three times a day) 50, 51, 79, 81 (The acetyl-l form of acetyl-carnitine crosses the blood/brain barrier and helps brain mitochondria as well)
- Creatine 50, 77, 78
- Folic acid 50, 79
- Malic acid (600-1200 mg twice a day) 2, 80, 81
Antioxidants for ROS
- Vitamin C (1000 mg twice a day) 28, 50, 51, 58, 73, 79
- Vitamin E (400-600 IU) 50, 51, 58, 73, 79
- Alpha-lipoic acid 28, 58, 66, 73, 79
- Vitamin B-6 74, 79
Recovery from prostration fatigue
- Vitamin B-1 (thiamine) (100 mg twice a day) 70, 50, 55, 79, 80
- Vitamin B-2 (riboflavin) (100 mg) 70, 50, 55, 79, 80
- Biotin (5 mg twice a day) 70, 55, 71, 75, 76, 79, 80
Postponing build-up of lactic acidosis
- Time-release guaifenesin (600-800 mg) 82
There is anecdotal evidence that guaifenesin slows the build-up of acidosis in skeletal muscles of ME/CFS patients who had enteroviruses or other skeletal-muscle attacking viruses as the trigger for their illness. Thus they have special extra damage to their skeletal muscles. Precisely why guaifenesin works is unknown, but it definitely does work for some patients. Guaifenesin is a uricosuric—a drug that increases the excretion of uric acid from the blood into urine. 83 It seems to help the excretion of excess phosphate from the cells of the body, which might have a bearing on mitochondrial dysfunction, since excess intracellular phosphate builds up with the hydrogen ion H+. 82, 83 Thus it might just act as a chemical buffer in the blood, slowing the build-up of acidity. The ME/CFS patient population that might be helped by this drug is a probably a small subset of the ME/CFS patient community.
Exercise and ME/CFS
Since ME/CFS patients get substantial bed rest and have excess cytokines which cause skeletal muscle destruction, as well as having the two types of fatigue mentioned above that create more muscle damage, it is important that ME/CFS patients get some exercise. However, typical physical therapy does not work, since the patients’ ability to safely exercise is limited. Any physical therapy that is undertaken has to be supervised by a physical therapist familiar with ME/CFS and the consequences of mitochondrial dysfunction with exercise. There are many studies showing that Graded Exercise Therapy (GET) can be very damaging to ME/CFS patients. 84 There is also anecdotal evidence that ME/CFS patients do not build up the muscle strength after exercise that a healthy person would.
Dr. Charles Lapp, an ME/CFS specialist at the Hunter-Hopkins Center, recommends, “Exercise no more than two to five minutes at a time and follow it up with five minutes of rest.” 85 It is essential that this sort of pacing while exercising is done so that more damage is not done and the two types of fatigue don’t develop.
Disclaimer for Patients
The various vitamins and supplements mentioned in this article have precautions, adverse reactions and side effects. Patients should check with their doctors before undertaking any part of the regimen suggested in the article. Patients also would be advised to read the article linked above, "Review of Nutritional Supplements Used for ME/CFS/FM" to note the general and specific cautions for a number of the supplements and vitamins reviewed in this article. As not enough is known about some of these supplements' effects on fetuses and babies, pregnant and lactating women should especially review the linked article as well as checking with their physicians before taking any of the cited vitamins or supplements.
References
- Berg CP et al, “Human Mature Red Blood Cells Express Caspase-3 and Caspase-8, but are Devoid of Mitochondrial Regulators of Apoptosis,” Cell Death Differ 8, no. 12 (2001): 1197-1206.
- Montgomery R et al, Biochemistry: A Case-Oriented Approach 3rd ed. St. Louis: C.V. Mosby Co., 1980.
- Wu I-C et al, “Metabolic Analysis of 13C-labeled Pyruvate for Noninvasive Assessment of Mitochondrial Function,” Annals NY Acad Sci 1201 (2010): 111-120.
- Adam-Vizi V, Chinopoulos C, “Bioenergetics and the Formation of Mitochondrial Reactive Oxygen Species,” Trends Pharmacol Sci.12 (2006): 639-45.
- Cadenas E, Davies KJ, “Mitochondrial Free Radical Generation, Oxidative Stress, and Aging,” Free Radic Biol Med. 29 no.3-4 (2000): 222-30.
- Lo M-C et al, “Glycoxidative Stress-induced Mitophagy Modulates Mitochondrial Fates,” Annals NY Acad Sci 1201 (2010): 1-7.
- Smith R, Murphy M, “Animal and Human Studies with the Mitochondrial-targeted Antioxidant MitoQ,” Annals NY Acad Sci 1201 (2010): 96-103.
- Wikipedia (2011). “Lactic acidosis.” http://en.wikipedia.org/wiki/Lactic_acidosis. Retrieved March 4, 2011.
- Hochachka PW, Mommsen TP, "Protons and anaerobiosis," Science 219 (1983): 1391–1397.
- Houten SM, Wanders RJA, “A General Introduction to the Biochemistry of Mitochondrial Fatty Acid β-oxidation,” J Inherit Metab Dis 33 (2010): 469-477.
- Foster DW, “The Role of the Carnitine System in Human Metabolism,” Annals NY Acad Sci 1033 (2004): 1-16.
- Berardo A et al, “A Diagnostic Algorithm for Metabolic Myopathies,” Curr Neurol Neurosci Rep 10, No. 2 (2010): 118-126.
- Famularo G et al, “Carnitines and its Congeners,” Annals NY Acad Sci 1033 (2004): 132-138.
- Schulz H, “Regulation of Fatty Acid Oxidation in Heart,”. J Nutr 124 (1994): 165–171.
- Howell N, “Human Mitochondrial Diseases: Answering Questions and Questioning Answers, Int Rev Cytol 186 (1999): 49-116.
- Zeviani M, Antozzi C, “Defects of Mitochondrial DNA,” Brain Pathol 2 No. 2 (1992): 121-132.
- Chavis JC (2009). “Who Discovered the Mitochondria?” http://www.brighthub.com/science/genetics/articles/26365.aspx. Retrieved March 13, 2011.
- Clay A et al, “Mitochondrial Disease,” Chest 120 (2001): 634-648.
- Wu C-L et al, “ Neuroprotective Mechanisms of Brain-derived Neurotrophic Factor Against 3-Nitropropionic Acid Toxicity: Therapeutic Implications for Huntington’s Disease,” Annals NY Acad Sci 1201 (2010): 8-12.
- Eastman P, “Investigators Focus on Mitochondrial Dysfunction Across the Life Spectrum,” Neurol Today April 15, 2010: 18-19.
- Adam-Vizi V, “Production of Reactive Oxygen Species in Brain Mitochondria: Contribution by Electron Transport Chain and Non-electron Transport Chain Sources,” Antioxid Redox Signal 7, no. 9-10 (2005): 1140-1149.
- Jung H S, Lee M-S, “Role of Autophagy in Diabetes and Mitochondria,” Annals NY Acad Sci 1201 (2010): 79-83.
- Wang C-H et al, “Mitochondrial Dysfunction in Insulin Insensitivity: Implication of Mitochondrial Role in Type-2 Diabetes,” Annals NY Acad Sci 1201 (2010): 157-165.
- Abdul-Ghani MA, DeFronzo RA, “Mitochondrial Dysfunction, Insulin Resistance and Type-2 Diabetes Mellitus,” Cur Diab Rep 8, No. 3, (2008): 173-178.
- Holloway G, “Mitochondrial Function and Dysfunction in Exercise and Insulin Resistance,” Applied Physiology, Nutrition and Metabolism June 1 (2009).
- Maassen JA, “Mitochondria, Fatty Acids, and Type-2 Diabetes Mellitus—What Is the Connection?” European Endocrine Disease Issue 2 (2006): 13-15. Retrieved from http://www.touchendocrinology.com/articles/mitochondria-fatty-acids-and-type-2-diabetes-mellitus-what-connection March 22, 2011.
- Sivitz W, Yorek M, “Mitochondrial Dysfunction in Diabetes: From Molecular Mechanisms to Functional Significance and Therapeutic Opportunities,” Antioxidants & Redox Signaling 12, no. 4 (2010): 537-579.
- Kim J et al, “Role of Mitochondrial Dysfunction in Insulin Resistance,” Circ Res 102, no. 4 (2008): 401-414.
- Peppa M et al, “ Skeletal Muscle Insulin Resistance in Endocrine Disease,” J Biomed Biotech (2010), Article ID 527850. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2840413/ March 22, 2011.
- Vermuelen R et al, “Patients with Chronic Fatigue Syndrome Performed Worse than Controls in a Controlled Repeated Exercise Study Despite a Normal Oxidative Phosphorylation Capacity,” J Translational Med 8 (2010): 93-100.
- Kennedy G et al, “Oxidative Stress Levels are Raised in Chronic Fatigue Syndrome and Are Associated with Clinical Symptoms,” Free Radical Biology and Medicine 39 (2005): 584-589.
- Paul L et al, “Demonstration of Delayed Recovery from Fatiguing Exercise in Chronic Fatigue Syndrome,” European Journal of Neurology 6 (1999): 63-69.
- Arnold D L et al, “Excessive Intracellular Acidosis of Skeletal Muscle on Exercise in a Patient with a Post-viral Exhaustion/Fatigue Syndrome,” Lancet 323, no. 8391 (1984): 1367- 1369.
- Behan WMH et al, “Mitochondrial Abnormalities in the Postviral Fatigue Syndrome,” Acta Neuropathologica 83, no. 1 (1991): 61-65.
- Plioplys AV, Plioplys S, “Electron-microscopic Investigation of Muscle Mitochondria in Chronic Fatigue Syndrome,” Neuropsychobiology 32, no. 4 (1995): 175-181.
- Plioplys AV, Plioplys S, “Serum Levels of Carnitine in Chronic Fatigue Syndrome: Clinical Correlates,” Neuropsychobiology 32, no. 3 (1995): 132-138.
- Kuratsine H et al, “Acylcarnitine Deficiency in Chronic Fatigue Syndrome,” Clin Infect Dis 18, Suppl 1 (1994): S62-S67.
- Lane RJ et al, “Heterogeneity in Chronic Fatigue Syndrome: Evidence from Magnetic Resonance Spectroscopy of Muscle,” Neuromuscul Disord 8, nos. 3-4 (1998): 204-209.
- Chazotte B, “Mitochondrial Dysfunction in Chronic Fatigue Syndrome,” Chapter 21. In Mitochondria in Pathogenesis, edited by Lemasters and Nieminen, 393-411. New York, NY: Kluwar Academic/Plenum Publishers, 2001.
- Myhill S et al, “Chronic Fatigue Syndrome and Mitochondrial Dysfunction,” Int J Clin Exp Med 2 (2009): 1-16.
- Nicholson G, Ellithorpe R, “Lipid Replacement and Antioxidant Nutritional Therapy for Restoring Mitochondrial Function and Reducing Fatigue in Chronic Fatigue Syndrome and Other Fatiguing Illnesses,” J CFS 13, no. 1 (2006): 57-68.
- Bazelmans E et al, “Impact of a Maximal Exercise Test on Symptoms and Activity in Chronic Fatigue Syndrome.” J Psychosom Res 59, no. 4 (2005): 201-208.
- Van Ness J et al, “Postexertional Malaise in Women with Chronic Fatigue Syndrome,” J Womens Health 19, no. 2 (2010): 239-244.
- Jammes Y et al, “Chronic Fatigue Syndrome: Assessment of Increased Oxidative Stress and Altered Muscle Excitability in Response to Incremental Exercise,” Journal of Internal Medicine 257 (2005): 299-310.
- VanNess J et al, “Diminished Cardiopulmonary Capacity During Post-Exertional Malaise,” J CFS 14, no. 2 (2007): 77-85.
- Wikipedia (2011). “ Muscle Fatigue.” http://en.wikipedia.org/wiki/Muscle_fatigue. Retrieved March 28, 2011.
- Sweet DE, “Metabolic Complications of Antiretroviral Therapy,” Top HIV Med 13, no. 2 (2005): 70-74.
- Lane RJM et al, “Muscle Fibre Characteristics and Lactate Responses to Exercise in Chronic Fatigue Syndrome,” J Neurol Neurosurg Psychiatry 64 (1998): 362-367.
- Roth SM, “Why does lactic acid build up in muscles? And why does it cause soreness?” Sci Amer Jan 23, 2006. http://www.scientificamerican.com/article.cfm?id=why-does-lactic-acid-buil. Retrieved March 28, 2011.
- DiMauro S et al, “Mitochondrial Encephalomyopathies: Therapeutic Approach,” Annals NY Acad Sci 1011 (2004): 232-245.
- Personal communication from Donald Johns, M.D. when he was chairperson of Neurology at Beth Israel-Deaconess Hospital in Boston, MA.
- Genova ML et al, “The Mitochondrial Production of Reactive Oxygen Species in Relation to Aging and Pathology,” Annals NY Acad Sci 1011 (2004): 86-100.
- Meng S-J, Yu L-J, “Oxidative Stress, Molecular Inflammation and Sarcopenia,” Int J Mol Sci 11 (2010): 1509-1526.
- Dinarello CA, “Interleukin 1 and Its Biologically Related Cytokines.” In Advances in Immunology Vol 44, edited by Frank Dixon, 153-205. New York, NY: Academic Press Inc, 1989.
- Dinarello CA, Cannon JG, “Interleukin 1.” In Progress in Immunology VI edited by B Cinader and RG Miller, 449-457. Orlando, FL: Academic Press Inc, 1986.
- Hendler SS and Rorvik D, editors. PDR for Nutritional Supplements, 1st edition. Montvale, NJ: Thomson PDR, 2001.
- Mukhopadhyay A, Weiner H, “Delivery of Drugs and Macromolecules to Mitochondria,” Adv Drug Deliv Rev 59, no. 8 (2007): 729-738.
- Smith RAJ et al, “Mitochondria-Targeted Antioxidants in the Treatment of Disease,” Annals NY Acad Sci 1147 (2008): 105-111.
- Jason LA et al, “The Energy Envelope Theory and Myalgic Encephalomyelitis/Chronic Fatigue Syndrome,” AAOHN J 56, no. 5 (2008): 189-195.
- Jason LA et al, “Provision of Social Support to Individuals with Chronic Fatigue Syndrome,” J Clin Psychol 66, no.3 (2010) : 249-58.
- Brown M et al, “The Role of Changes in Activity as a Function of Perceived Available and Expended Energy in Nonpharmacological Treatment Outcomes for ME/CFS,” J Clin Psychol 67, no. 3 (2011):253-60.
- Jason LA, Benton M, “The Impact of Energy Modulation on Physical Functioning and Fatigue Severity Among Patients with ME/CFS,” Patient Educ Couns 77, no. 2 (2008): 237-241.
- Personal observation by the author, who has had CFS/ME since 1957.
- Jason LA et al, “CFS Prevalence and Risk Factors over Time,” Health Psychol 11 ( 2011) epub.
- Friedberg F et al, “Symptom Patterns in Long-Duration Chronic Fatigue Syndrome,” J Psychosomatic Research 48 (2000): 59-68.
- Singh U, Jialil I, “Alpha-Lipoic Acid Supplementation and Diabetes,” Nutr Rev 66, no. 11 (2008): 646-657.
- Morré D et al, “Surface Oxidase and Oxidative Stress Propagation in Aging,” J Experimental Biol 203 (2000): 1513-1521.
- Maes M et al, “Coenzyme Q10 Deficiency in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) is Related to Fatigue, Autonomic and Neurocognitive Symptoms and is Another Risk Factor Explaining the Early Mortality in ME/CFS Due to Cardiovascular Disorder,” Neuro Endocrinol Lett 30, no.4 (2009): 470-6.
- Kowaltowski AJ, Vercesi AE., “Mitochondrial Damage Induced by Conditions of Oxidative Stress,” Free Radic Biol Med 26, no.3-4 (1999): 463-71.
- Personal communication from Fred Hochberg, MD, a neurologist at Massachusetts General Hospital, Boston and professor of the Harvard Medical School.
- Killilea DW, Ames BN, “Magnesium Deficiency Accelerates Cellular Senescence in Cultured Human Fibroblasts,” Proc Natl Acad Sci USA 105 (2008): 5768-5773.
- Bonakdar RA, Guarneri E, “Co-Enzyme Q-10,” Am Fam Physician 72, no.6 (2005): 1065-1070.
- Wray DW et al, “Antioxidants and Aging: NMR-based Evidence of Improved Skeletal Muscle Perfusion and Energetics,” Am J Physiol Heart Circ Physiol 297 (2009): H1870-H1875.
- Choi E-Y, Cho Y-O, “Effect of Vitamin B-6 Deficiency on Antioxidative Status in Rats with Exercise-Induced Oxidative Stress,” Nutrition Res Practice 3, no. 3 (2009): 208-211.
- Wolf B, Feldman GL, “The Biotin Dependent Carboxylase Deficiencies,” Am J Hum Genet 34 (1982): 699-718.
- Roth KS, “Biotin in Clinical Medicine,” Am J Clin Nutri 34 (1981): 1967-1974.
- Adhihetty PJ, Flint MF, “Creatine and Its Potential Therapeutic Value for Targeting Cellular Energy Impairment in Neurodegenerative Diseases,” Neuromolecular Med 10, no. 4 (2008): 275-290.
- Young JF et al, “Creatine-Induced Activation of Antioxidative Defense in Myotube Cultures Revealed by Exploratory NMR-based Metabomics and Proteomics,” JISSN 2010: 7-9.
- Naviaux R, “A Primary Care Physician’s Guide: The Spectrum of Mitochondrial Disease,” Exceptional Parent Magazine 27, no. 8 (1997). Retrieved from http://biochemgen.ucsd.edu/mmdc/ep-3-10.pdf on March 31, 2011.
- Anecdotal evidence from CFS/ME patients and description of information from the PDR as explained in our article "Review of Nutritional Supplements Used for CFS/ME/FM."
- Recommended by Charles Lapp MD and other ME/CFS specialists as explained in our article "Supplements."
- St. Amand P, “The Use of Guaifenesin in Fibromyalgia,” Fibromyalgia Treatment Center, http://www.fibromyalgiatreatment.com/Uricosuric%20 June%202009.pdf. Retrieved April 3, 2011.
- Wikipedia (2011). “Guaifenesin.” http://en.wikipedia.org/wiki/Guaifenesin Retrieved April 3, 2011.
- Maes M, Twisk FNM, “Chronic Fatigue Syndrome: Harvey and Wessley’s (Bio)psychosocial Model Versus a (Bio)psychosocial Model Based on Inflammatory and Oxidative and Nitrosative Stress Pathways,” BMC Medicine 8 (2010): 35-48.
- Lapp C, “Stepwise Approach to Fibromyalgia and Chronic Fatigue Syndrome,” Pro Health Library 2002. http://www.prohealth.com/library/showarticle.cfm?id=3714&t=CFIDS_FM Retrieved April 3, 2011.
Health care providers might also want to consult the 2014 ME/CFS: A Primer for Clinical Practitioners.
